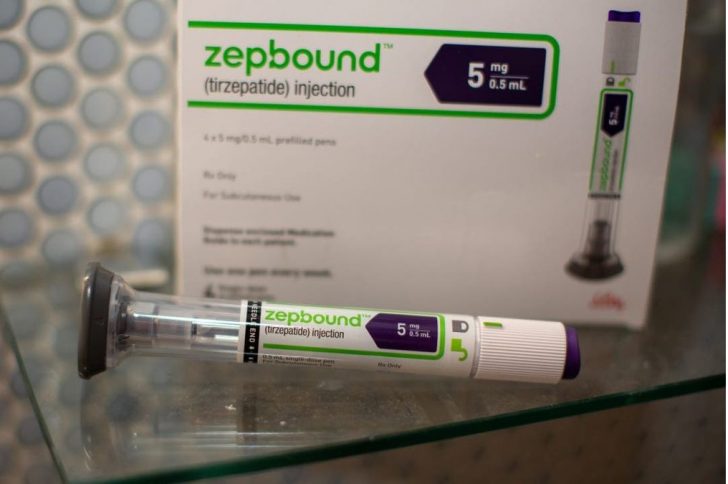
The FDA has approved Zepbound, a prescription medication for treating moderate to severe obstructive sleep apnea (OSA) in people with obesity. This groundbreaking approval highlights the potential for GLP-1 receptor agonists, such as Zepbound, to address dual health concerns. Alongside a reduced-calorie diet and increased physical activity, Zepbound offers a novel approach to managing OSA, a condition that disrupts sleep and poses significant health risks.
Understanding Obstructive Sleep Apnea and Obesity
OSA affects nearly 30 million Americans and often goes undiagnosed. The condition is characterized by blocked airflow during sleep, causing breathing disruptions that may result in daytime fatigue, snoring, and gasping. Obesity significantly increases the likelihood of OSA, and weight loss can alleviate its severity. Untreated OSA raises the risk of cardiovascular and neurological complications, underscoring the need for effective treatment options.
Zepbound: A Multifunctional Treatment for OSA and Weight Loss
Zepbound, initially approved in 2023 for weight management, now serves a dual purpose. It aids in weight loss while reducing symptoms of OSA. Clinical trials revealed that nearly half of the participants experienced symptom relief to the extent they no longer met the diagnostic criteria for OSA. This transformative impact reflects the drug’s ability to target the root causes of both conditions.
Clinical Trial Insights: Zepbound’s Impact on OSA
The FDA's approval was based on two key trials involving approximately 470 participants. These studies assessed Zepbound's effects on the apnea-hypopnea index (AHI), a metric measuring breathing disruptions per hour. Participants had an average baseline AHI of about 50 events per hour and a body mass index (BMI) of 39, highlighting the severity of their condition.
In patients not using CPAP machines, Zepbound reduced AHI events by 25 per hour, compared to just five with placebo. In CPAP users, Zepbound decreased events by 29 per hour, compared to six with placebo. These results demonstrate the drug’s efficacy across different treatment contexts.
Additional Benefits of Zepbound Beyond Sleep Apnea
Beyond reducing AHI events, Zepbound led to significant weight loss, with participants shedding 18% to 20% of their body weight over a year. This equates to an average of 45 to 50 pounds. The medication also improved cardiovascular health markers, such as blood pressure and inflammation, which are critical in managing OSA-related risks. These multifaceted benefits position Zepbound as a valuable tool in comprehensive obesity and OSA management plans.
Financial Accessibility and Insurance Implications
Zepbound's approval could expand its accessibility for individuals with OSA, particularly those reliant on Medicare. Medicare currently limits coverage of weight-loss medications unless prescribed for another condition, like OSA. While the drug costs $1,060 per month, Eli Lilly offers discounts and alternative administration methods to reduce expenses. These options make the treatment more feasible for a broader patient population.

@lifemd | Instagram | Zepbound's approval expands its accessibility for individuals with obstructive sleep apnea.
Side Effects and Safety Considerations
The most common side effects of Zepbound include gastrointestinal symptoms, which are typically mild to moderate. These effects occur primarily during the initial stages of treatment or when doses are increased. The safety profile aligns with other GLP-1 receptor agonists, making it a manageable option for most patients.
Zepbound represents a significant advancement in addressing OSA and its associated health risks. The drug’s ability to simultaneously target obesity and improve sleep quality underscores its transformative potential for millions of Americans struggling with these conditions.